INS LifeGuard
The Impact of Alzheimer’s Disease in Australia

Alzheimer’s disease and other forms of dementia affect a significant portion of the Australian population, making it a growing public health challenge. As of 2023, approximately 411,100 Australians are living with dementia, and Alzheimer’s disease is the most common cause. This includes nearly 257,500 women and 153,700 men, highlighting its widespread impact across genders.
The likelihood of developing dementia increases with age:
- Around 1 in 12 people aged 65 and older are affected.
- This rises to a staggering 2 in 5 Australians aged 90 and over.
People with Alzheimer’s disease are expected to climb sharply in the coming decades as Australia’s population ages. By understanding the prevalence and addressing it proactively, we can help individuals and families navigate the challenges of Alzheimer’s disease with greater confidence and support.
Alzheimer’s disease has profound implications for individuals, families, and caregivers worldwide. This guide delves into key aspects of Alzheimer’s disease to promote awareness, early detection, and effective management.
What Is Alzheimer’s Disease?
How Alzheimer’s Disease Differs from Other Forms of Dementia Symptoms
Dementia is a broad term for conditions that involve cognitive decline, but Alzheimer’s disease stands out due to its specific underlying changes in the brain. It is characterised by pathological markers, including:
- Amyloid plaques: Sticky clumps of protein that build up between nerve cells, blocking communication.
- Tau tangles: Twisted fibres inside nerve cells that disrupt the flow of nutrients and essential signals.
These abnormalities damage and eventually kill brain cells, leading to the hallmark symptoms of Alzheimer’s disease: memory loss, confusion, and cognitive decline. Unlike normal aging, this process is not an inevitable part of growing older but results from a combination of genetic, environmental, and lifestyle factors.
Other forms of dementia differ in their causes and progression:
- Vascular dementia results from reduced blood flow to the brain, damaging brain cells and impairing cognitive function.
- Lewy body dementia involves abnormal protein deposits in brain cells, affecting thinking, movement, and mood.
Understanding Alzheimer’s Disease
Alzheimer’s disease is the most common type of dementia, but it is also a complex and multifaceted condition. Alzheimer’s disease process gradually impairs cognitive function; the most common early symptoms include mild memory loss before advancing to severe mental and physical disabilities.
A defining feature of Alzheimer’s disease is the buildup of two types of proteins in the brain: beta-amyloid and tau. These proteins accumulate to form plaques and tangles, disrupting normal brain function and leading to the widespread loss of brain cells over time.

This progressive damage for people with Alzheimer’s disease affects memory, thinking, and behaviour, making early detection and management critical for improving quality of life and planning for care.
Causes and Risk Factors of Alzheimer’s Disease
Multiple factors influence the development of Alzheimer’s disease:
Genetic Factors and Alzheimer’s Disease Risk
Certain genetic variations can increase the likelihood of developing Alzheimer’s disease. One of the most well-studied genes linked to Alzheimer’s disease is APOE (Apolipoprotein E), which comes in several forms.
APOE-ε4
This particular variant significantly raises the risk of Alzheimer’s disease. People who inherit one copy of the APOE-ε4 gene from a parent have an increased risk, while those with two copies (one from each parent) face an even higher likelihood of developing the disease.
Who is most likely to have APOE-ε4?
While anyone can carry this gene, it is more commonly found in individuals with a family history of Alzheimer’s disease. However, having APOE-ε4 does not guarantee someone will develop Alzheimer’s disease, nor does its absence eliminate the risk.
In rare cases, Familial Alzheimer’s Disease (FAD) is caused by specific mutations in other genes, such as APP, PSEN1, and PSEN2, which lead to early-onset Alzheimer’s disease (before age 65). This form of the disease is hereditary and often affects multiple generations.
Additionally, individuals with Down Syndrome are at a much higher risk of developing Alzheimer’s disease due to an extra copy of chromosome 21, which carries the gene for the amyloid precursor protein (APP). This increases the production of amyloid plaques, a hallmark of Alzheimer’s disease.
The Role of Environmental Risk Factors in Alzheimer’s Disease
Specific environmental exposures can increase the likelihood of developing Alzheimer’s disease by affecting brain health over time. Key factors include:
Air Pollution
Long-term exposure to delicate particulate matter (PM2.5) in air pollution has been linked to an increased risk of dementia. Pollutants may cause inflammation in the brain and damage brain cells.
Toxins
Exposure to harmful substances, such as heavy metals (e.g., lead or mercury) or industrial chemicals, may have neurotoxic effects that contribute to cognitive decline.
Traumatic Brain Injuries (TBI)
Head injuries, especially repeated or severe trauma, can significantly increase the risk of Alzheimer’s disease and other forms of dementia. TBIs may trigger abnormal protein buildup in the brain, such as tau tangles, that disrupt brain function.
Reducing environmental exposures where possible, such as improving air quality at home or using protective equipment in hazardous workplaces, may help lower the risk of Alzheimer’s disease.
How Lifestyle Choices Influence Alzheimer’s Disease Risk
Everyday habits and routines play a crucial role in brain health, and certain lifestyle factors are known to elevate Alzheimer’s disease risk:
Unhealthy Diets
Diets high in processed foods, refined sugars, and saturated fats may contribute to inflammation and oxidative stress, which harm brain cells. Conversely, a healthy diet, particularly a Mediterranean diet rich in fruits, vegetables, whole grains, fish, and healthy fats, has reduced the risk.
Lack of Physical Activity
Regular aerobic exercise improves blood flow to the brain, reduces inflammation, and promotes the release of neuroprotective compounds. Sedentary lifestyles are associated with poorer cognitive outcomes.
Smoking
Smoking accelerates oxidative stress and vascular damage, increasing the risk of both vascular dementia and Alzheimer’s disease.
Insufficient Mental Stimulation
Keeping the brain active through learning, puzzles, reading, or social engagement helps build a healthy brain and cognitive resilience. A lack of mental challenges over time can contribute to cognitive decline.
Managing Stress and Anxiety
Chronic stress can negatively impact cognitive function, so finding ways to manage stress is crucial.
Getting Enough Sleep
Quality sleep is essential for brain health and can help reduce the risk of cognitive decline.
Managing Chronic Health Conditions
Conditions like diabetes and high blood pressure can increase the risk of Alzheimer’s disease, so managing these conditions is essential.
Research has also shown that certain medications and supplements may help reduce the risk of developing Alzheimer’s disease and dementia symptoms and improve overall brain health. These include cholinesterase inhibitors, which can improve cognitive function and memory, and memantine, which can slow disease progression. Omega-3 fatty acids and vitamin D have also been shown to support brain health and reduce the risk of cognitive decline.
Role of Age and Family History
Age
Alzheimer’s disease risk increases significantly after age 65, with nearly one-third of individuals aged 85 or older affected.
Family History
Having a close relative with Alzheimer’s disease increases your likelihood of developing the disease, especially if genetic factors are involved. Familial Alzheimer’s disease, a rare form typically beginning in the 50s, is genetically inherited and often affects multiple family members across generations.
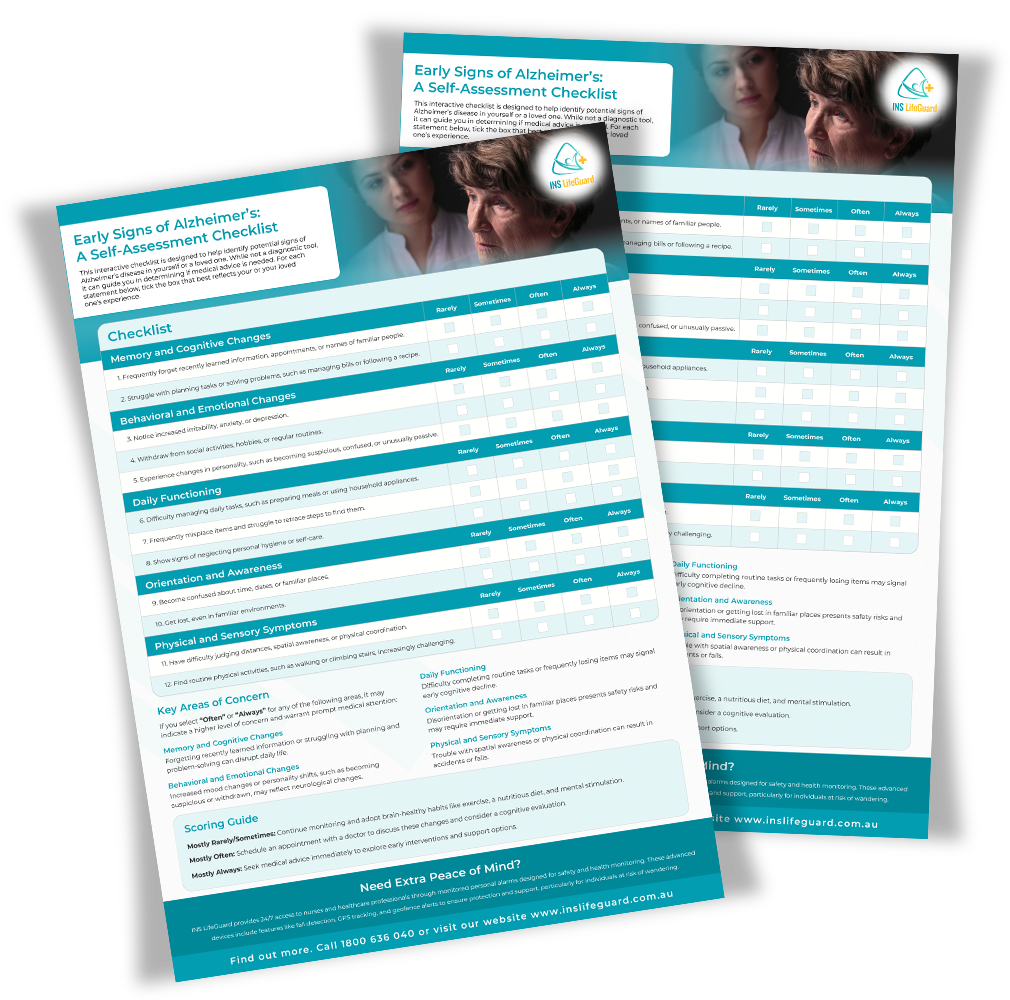
Early Signs and Symptoms of Mild Cognitive Impairment
Identifying Cognitive and Behavioral Changes
Memory Loss
Memory problems and forgetting recently learned information, appointments, or names of familiar people.
Difficulty Planning or Problem-Solving
Struggling with tasks such as managing finances or following a recipe.
Confusion
Disorientation regarding time, place, or familiar environments.
Behavioural Changes
Increased irritability, depression, or withdrawal from social activities. Dementia symptoms worsen over time, affecting daily activities and independence.
Early Symptoms of Alzheimer’s: A Self-Assessment Checklist
Early detection is key to effectively managing Alzheimer’s disease. To help you stay proactive, we have created an easy-to-use downloadable resource to help you or your loved ones identify potential symptoms of Alzheimer’s disease and take the following steps toward support and care.
Importance of Early Diagnosis
Early detection of Alzheimer’s disease facilitates better management and allows for planning and access to clinical trials. Treatments initiated early may slow the disease’s progression and improve quality of life but will not cure it. The process of getting Alzheimer’s disease diagnosed involves a thorough examination, including discussions about symptoms and medical history, as there is no single confirmatory test.
Symptoms and Stages
The symptoms of Alzheimer’s disease can vary widely among individuals, but they often include memory loss, confusion, difficulty with communication, and changes in mood and behaviour. In the early stages, symptoms may be mild cognitive impairment, and early symptoms may not be immediately noticeable to others. As Alzheimer’s disease progresses, these symptoms become more pronounced and begin to interfere with daily life.
Alzheimer’s disease is generally categorised into three stages as Alzheimer’s disease progresses:
Early stage
Mild Alzheimer’s Disease
At the early stage of Alzheimer’s disease, individuals may experience memory loss, difficulty with problem-solving, and subtle changes in mood and behaviour. These symptoms can be easily overlooked or attributed to normal aging.
Middle stage
Moderate Alzheimer’s Disease
As Alzheimer’s disease progresses, symptoms start to become more noticeable. These may include difficulty with everyday tasks such as bathing, dressing, and managing finances. Changes in personality and increased confusion are common during this stage.
Late stage
Severe Alzheimer’s Disease
In this stage, people with Alzheimer’s disease may have significant difficulty with communication, experience trouble swallowing, and lose motor skills. They often have severe symptoms requiring full-time care and assistance with all aspects of daily living.
Diagnosis and Assessment
Medical Tests and Cognitive Evaluations for Alzheimer’s Disease
Cognitive Tests
Evaluate memory, attention, problem-solving, and language abilities. Examples include the MMSE (Mini-Mental State Examination).
Imaging Tests
MRI and CT scans help rule out other causes of cognitive decline, while PET scans identify amyloid plaques.
Biomarkers
Testing cerebrospinal fluid or blood for tau and amyloid proteins is emerging as a powerful diagnostic tool. However, there is no single definitive test to diagnose Alzheimer’s disease, and careful assessment by medical specialists is necessary.
How to Prepare for a Doctor’s Visit
- Keep a journal of symptoms, noting when and how they’ve changed.
- Bring a complete medical history, including medications and a family history of dementia.
- Prepare questions about tests, treatment options, and caregiving resources. As people develop Alzheimer’s disease, symptoms deteriorate over time, leading to a significant loss of independence and increased behavioural challenges.
Alzheimer’s Disease Management and Treatment Options
Current Alzheimer’s Disease Medications and Their Effects
Cholinesterase Inhibitors (e.g., donepezil, rivastigmine)
These drugs enhance communication between nerve cells by increasing acetylcholine levels, offering temporary symptom relief. Being diagnosed with Alzheimer’s disease can have significant implications, as early detection allows for timely intervention and management.
Memantine
Helps moderate to advanced Alzheimer’s disease by regulating glutamate activity and preventing overstimulation of nerve cells. As the disease progresses to moderate Alzheimer’s, there is an increased need for daily support, with patients facing specific challenges in maintaining their independence.
Emerging Therapies and Clinical Trials
Anti-Amyloid Treatments
Drugs like lecanemab aim to clear amyloid plaques from the brain. Acetylcholinesterase inhibitors and memantine play a crucial role in the treatment of severe or advanced Alzheimer’s disease, helping manage cognitive symptoms and improving quality of life.
Gene Therapy
Research explores how to modify genes linked to Alzheimer’s disease risk factors.
Lifestyle Interventions
Studies show the effectiveness of combining diet, exercise, and cognitive training.
Caregiving Tips for Alzheimer’s Disease
Strategies for Effective Communication
- Speak clearly and slowly, using simple sentences.
- Maintain eye contact and use nonverbal cues to reinforce understanding.
- Validate emotions rather than correcting memory lapses.
- Information from family members can help caregivers understand the patient’s daily living abilities and mental function.
Managing Behavioral Changes and Challenges
- Identify triggers for agitation or aggression and create a calming environment.
- Use distractions or activities to redirect attention from distressing situations.
Tips for Self-Care as a Caregiver
- Build a support network of friends, family, and professional caregivers.
- Prioritise your mental health with counselling or relaxation techniques.
- Access respite care services to avoid burnout.
Daily Living Aids and Safety
Living with Alzheimer’s disease presents unique challenges, but the right tools and modifications can significantly enhance safety and independence.
Technology and Tools for Independence
GPS Trackers
Provide safety for individuals prone to wandering by ensuring they can be quickly located.
Fall Detection Systems
Automatically detect falls and send alerts to emergency support or caregivers, ensuring timely help even if the individual cannot call for assistance.
Personal Alarms
Allow users to quickly call for help with the press of a button, offering peace of mind for those with Alzheimer’s disease and their loved ones.
Reminder Devices
Simplify daily routines with automated prompts for medications, meals, or appointments.
Voice Assistants
Support daily tasks by offering reminders, answering questions, and controlling home devices.
Home Modifications for Safety and Accessibility
- Install grab bars in key areas like bathrooms and hallways to provide extra support and prevent falls.
- Secure rugs and loose carpets to reduce tripping hazards.
- Locks on cabinets containing hazardous items like cleaning products or medications should be used.
- Add
motion-sensor lighting to improve visibility, especially at night.

By combining technology, daily living aids, and home modifications, caregivers can create a safer environment that promotes independence and dignity for individuals living with Alzheimer’s disease.
Living with Alzheimer's Disease
Living with Alzheimer’s disease presents many challenges, but numerous resources are available to help individuals and their families navigate this journey. Support groups can provide emotional support and a sense of community, while home care services can assist with daily activities and help maintain independence. Adult daycare programs offer socialisation and activities during the day, and respite care provides temporary relief for caregivers.
Online resources and educational materials can offer valuable information and guidance on managing the disease. It’s important to remember that people with Alzheimer’s disease can still live fulfilling and meaningful lives. With the proper support and care, it is possible to manage the symptoms of Alzheimer’s disease and maintain independence for as long as possible.
Coping with a Diagnosis
Emotional Support for Individuals and Families
- Seek counselling or therapy to process feelings of grief and anxiety.
- Encourage open conversations about the diagnosis and plans. Early onset Alzheimer’s disease, which typically affects individuals in their 40s or 50s, presents unique challenges and characteristics.
Addressing Stigma and Misunderstandings
- Educate friends and communities to reduce fear and misconceptions about Alzheimer’s disease.
- Advocate for inclusivity and understanding in public spaces.
Support Networks and Resources
- Join organisations like the Alzheimer’s Association or Dementia Australia for peer support and educational resources.
- Participate in online forums for tips, encouragement, and shared experiences. As the disease progresses, people with Alzheimer’s disease increasingly depend on caregivers, making support networks crucial.
Professional Organisations Offering Help
- Access helplines, home care services, and respite care options.
Dealing with Grief and Loss
- Recognise feelings of grief as the person with Alzheimer’s disease changes due to cognitive decline.
- Seek therapy to process these complex emotions and adapt to evolving relationships.
Research, Advocacy, and Emerging Technologies in Alzheimer’s Disease Care
Advances in Biomarkers, Imaging, and Therapies
Recent breakthroughs in Alzheimer’s research have paved the way for earlier and more accurate diagnoses. Blood tests for amyloid and tau proteins now allow healthcare providers to identify developing Alzheimer’s disease in its initial stages, improving treatment opportunities. Additionally, new brain scans and imaging technologies enable better tracking of disease progression, giving researchers and clinicians deeper insights into the condition.
Promising Breakthroughs in Early Detection
Innovative tools are being developed to identify subtle signs of Alzheimer’s disease before noticeable symptoms appear. AI-powered systems analyse speech patterns, movement, and other behaviours, offering a non-invasive approach to early detection. Genetic risk assessments are also gaining traction, helping identify individuals who could benefit from early interventions.
Innovative Technologies for Alzheimer’s Care
Emerging technologies are transforming the way Alzheimer’s disease is managed and treated. For example:
Virtual Reality (VR)
VR experiences are being used to stimulate memory and cognitive functions, helping individuals with Alzheimer’s disease engage in meaningful activities.
Smart Home Systems
These systems automate reminders for safety, daily activities, and medication schedules, promoting independence.

The Future of Assistive Tech in Dementia Care
As technology advances, assistive devices are becoming increasingly personalised and proactive, revolutionising care for individuals with Alzheimer’s disease. Solutions like the INS LifeGuardian® App, when paired with a smartwatch, provide cutting-edge predictive health monitoring and tailored care recommendations. INS LifeGuard’s nurses and other health care professionals monitor these wearable technologies seamlessly, tracking vital signs and physical activity while offering advanced features such as fall detection, GPS tracking, and geofence boundaries to enhance safety and peace of mind.
The free INS LifeGuardian Connect® app for iOS and Android also allows families and carers to stay connected and involved. With the INS LifeGuardian Connect® app, carers can track and monitor loved ones in real time, set alerts, and manage health updates conveniently via their smartphones. These innovative solutions ensure comprehensive support and empower caregivers to provide the best care possible.
This guide offers a comprehensive view of Alzheimer’s disease, from understanding its progression to exploring the latest advancements in treatment and care. By taking proactive steps and utilising the right tools, you can enhance safety, independence, and quality of life for individuals affected by Alzheimer’s disease. Discover how INS LifeGuard's cutting-edge personal alarms, fall detection systems, and TeleHealth services can support individuals and caregivers in managing Alzheimer’s disease effectively. Visit our website today or call
1800 636 040 to speak to a friendly staff member and to learn more.
New paragraph

About
INS LifeGuard is the only 24/7 nurse on-call personal and medical monitoring in Australia. We provide monitoring technology for both in the home and on the go and can also monitor other provider's equipment. Our services are suitable for anyone wanting support to stay independent such as the elderly, those with medical conditions and disabilities plus enhancing safety and security for lone workers.